
Rosacea Treatment Procedures in Singapore
- March 31, 2022


Looking in the mirror can be aggravating when all that you see is your red skin, visible blood vessels, and sometimes even bumps and lumps looking right back at you. That is, if your rosacea hasn’t made your eyes watery enough to actually see the mirror clearly. Having rosacea is no fun at all – a survey conducted by the National Rosacea Society involving more than 400 patients with rosacea revealed that 75% of respondents reported that their rosacea had lowered their self-esteem, made them feel embarrassed (70%), frustrated (69%), and more than 50% of respondents also said that they felt robbed of pleasure or happiness because of their rosacea.
The current ways of treating rosacea focus mainly on reducing and managing symptoms in a way that reduces the number and intensity of flare ups, as well as identifying the main factors in preventing rosacea. Preventing rosacea flare ups can help to improve the sufferer’s quality of life, prevent progression of the disease, and to maintain a state of remission where the frequency of flare ups stay quiet for longer. But what else can be done? This article will go through three available rosacea treatment procedures in Singapore.
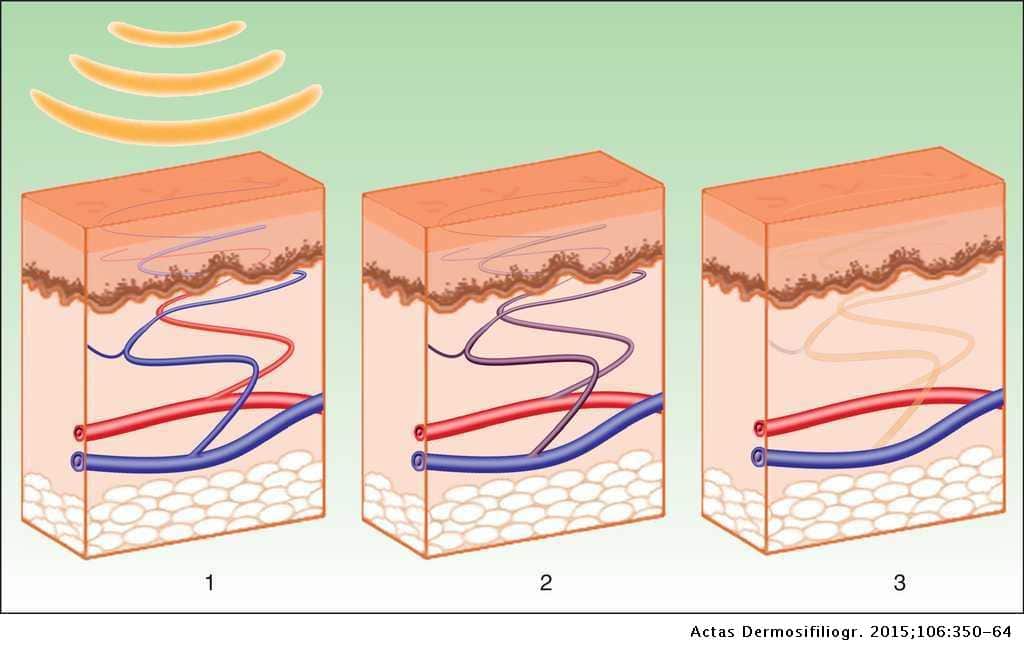
Rosacea treatment in Singapore often include laser treatment procedure, or pulsed light therapy. This mainly aims to target very visible blood vessels which contribute to excessive flushing. Laser treatments can work two ways: Using heat to ‘cauterise’ or ‘collapse’ the blood vessels, or using a non-heat version to break up the red patches.
Such lasers can be the Q-switched ND:YAG laser or pulsed laser therapy like the Pico Laser and the Fotona Laser, although several sessions over a period of time are needed to see results. Some studies which support the use of laser are:
Some side effects in those studies reported were of hyperpigmentation, a period of rosacea exacerbation, or bruising after the procedure. Hence, the suitability of candidates is important. Very inflamed skin may require the use of oral or topical medication first before undergoing laser therapy to prevent the occurrence of these side effects.
Electrosurgery uses a different method to address the visible blood vessels or excessive tissue growth because of rosacea (phymatous rosacea). This procedure involves the insertion of a very thin needle into the surface of the skin. A carefully selected electric current is used via the needle to target those blood vessels or excess tissue, which respond by clotting (blood coagulation) and shrinking. A scab will form over the treated areas which will eventually fall off on its own, leaving behind a smaller area of previously symptomatic skin.

This method is typically used for rhinophyma, the excessive growth of skin tissue over the nose regions in men who have phymatous rosacea. This is because it can cause scarring, especially when used over larger areas.
A review on the treatment methods available for such symptoms have found that laser treatment usually produces an equal cosmetic result when compared to electrosurgery, making laser a preferred choice due to less risk of scarring.

Dermabrasion does not involve lasers or electric current. Instead, the name dermabrasion is from the combination of ‘dermal’ and ‘abrasion’ – the exfoliation and removal of the superficial layer of your skin through non-surgical methods. Typically, tiny crystals are used to break up the skin cells to reveal the smoother skin underneath. Some patients with rosacea also have very sensitive skin, especially those experiencing the erythematotelangiectatic (ETR) or papulopustular (PPR) subtype of rosacea. Hence, dermabrasion is often used for phymatous rosacea; however, similar to electrosurgery, dermabrasion runs the risk of scarring after the procedure. The dermabrasion acts to ‘sand down’ the upper layers of excessive skin tissue and encourage new and smoother skin cells to replace the area.
Again, it can be said that other more suitable treatment techniques like oral or topical anti-inflammatory medication and the use of laser can provide excellent results with less risk of harmful side effects in rosacea patients. The consultation of a dermatologist is important to identify which treatment works best for you.
Have you heard of ‘Ivermectin’ before? You definitely might have, as it became viral during the COVID-19 pandemic as a form of ‘miracle drug’ against COVID-19 symptoms although it is actually a vital anti-parasitic medicine used to treat humans and animals. Surprisingly, a form of Ivermectic cream which is prescription-only called Soolantra is used in the treatment of rosacea – and, unlike its use in COVID-19, the use of Soolantra in rosacea is actually verified to reduce the population of Demodex mites on the surface of the skin which can contribute to rosacea flares.
For those who need to bring down the inflammatory lesions, such as in papulopustular rosacea (PPR), this topical prescription cream may help symptoms before other laser treatments are considered.
Stromectol may be used as an adjunct in the treatment of rosacea by reducing the number of Demodex mites in the skin, thereby reducing inflammation and improving the control of rosacea.
Absolutely. Other than the unwanted social effects of feeling embarrassed or frustrated, the physical symptoms of burning, itching, and sensitive skin can be equal cause to treat rosacea. Untreated rosacea can get worse over time because of chronic inflammation of the blood vessels – the skin layer tends to become thinner, more sensitive, and with more visible blood vessels.
We understand that treating rosacea can be a long process to find a treatment that works for you. If you’d like to come in for a consultation on procedure of rosacea treatment in Singapore to assess if you are suitable for a specific treatment, book an appointment today with SL Aesthetic.
Like what you read? Share them!