


You know the feeling all too well… Your face begins to flush and you feel the heat creeping up from your neck to your cheeks. When you look in the mirror, what pops out is the rough texture of your skin and enlarged pores, highlighted even more when accompanied with with the redness from flushing. That’s rosacea, and you’re having a flare. And if you’re lucky, this flare won’t be followed by more bumps or pus-filled pustules on your chin and cheeks – if you’re unlucky, this flare will last for days or weeks and contribute to the skin thickening that you might be experiencing anywhere along not just your cheeks and chin, but your forehead, nose, eyelids, and even ears.
We all know that nobody wants rosacea. But why exactly does it appear? This article will dive into the many common causes of rosacea including interesting things like mites and bacteria to give you a comprehensive understanding of what causes rosacea.
There are several common causes of rosacea, ranging from the commonly known ones to the rare ones.
The first is genetics, because that involves all that you’ve inherited from your immediate and close family members all the way to your far ancestry – it might just be in your blood. There is usually a positive family history for rosacea, although this was minimally proven until recently. In 2015, genome-wide association studies that involved rapidly scanning markers across complete sets of DNA of many people were conducted to find a link between genes and rosacea, which they did! Several genes that they identified could be passed on through genetics, and also has a close link to the immune system.
Those genes mentioned in, were actually variants of a particular DNA sequence in two genes: The butyrophilin-like (BTNL2) gene, and the human leukocyte antigen–DRA (HLA-DRB1) genes. These two genes are closely related to the immune system which indicates that dysregulations of the immune system have a role to play in rosacea. This makes sense because the redness and tenderness in rosacea is inflammation which is triggered by an immune system response.
For rosacea that causes granulomatous changes – e.g. lumps and bumps on the skin, such as in papulopustular rosacea or phymatous rosacea – another study found the influence of the NOD2/CARD15 gene. This gene is also associated with the function of the automatic immune system and also in subsequent inflammatory processes. Hence, it doesn’t come as a surprise that the DNA that codes for rosacea also shares a genetic risk loci with various other auto-immune diseases such as multiple sclerosis, celiac disease, type 1 diabetes, and rheumatoid arthritis. A genetic risk loci means that the position of the chromosomes that contribute to those conditions lie within the same region.
What these two first points mean is that when rosacea previously couldn’t be pinpointed to a genetic trait, science now shows that there is a factor of inheritance involved, which also may make a person more susceptible to other autoimmune diseases. Knowing this can increase awareness to both medical practitioners and rosacea sufferers to keep an eye out for those at risk of developing other autoimmune disorders!
And it’s not just what you’ve inherited from your parents or grandparents either. DNA can be traced all the way back to our ancestors, and that can be said for rosacea as well.

If you do a quick search on rosacea and ancestry, you’ll find plenty of results that tell you that Celtic and Scandinavian ancestry might be more at risk of passing on rosacea. But why? Studies into why Celtic or Nordic blood might have a higher risk of rosacea shows that it’s actually an evolutionary advantage! So, not as much of a curse as it is a blessing.
Back then during the long Nordic winters, ultraviolet levels were very low from reduced sun exposure. A gene called CAMP (cathelicidin antimicrobial peptide) which plays a crucial role in antimicrobial defences such as the killing of mycobacteria could not be activated because it needs Vitamin D, which was lacking. The Celts then eventually acquired a mutation that activates an alternative to express the CAMP gene through pathways that don’t require Vitamin D.
However, although those Vitamin D-independent pathways helped against bacterial defence, it had one big con – it encouraged other genetic factors that mediate immune reactions and which increase endoplasmic reticulum (ER) stress responses. At the molecular level, all trigger factors for rosacea can be regarded as ER stressors. This genetic ‘mutation’ was then passed down through the Celtic or Nordic genes, and makes the ancestors of these long winter survivors more susceptible to rosacea.
Aside from these Scandinavian ancestries, there is also a prevalence of rosacea in some Asian communities! This can be due to variations in skin pigmentation across different types of Asian ethnicities, which range from melanin-rich skin to those who have very fair skin that burns easily in the sun. It is usually those who are very fair skin and are sensitive to UV rays that experience the negative effects of rosacea more, due to poor defences against UV radiation which is a big trigger for redness and visible blood vessels.
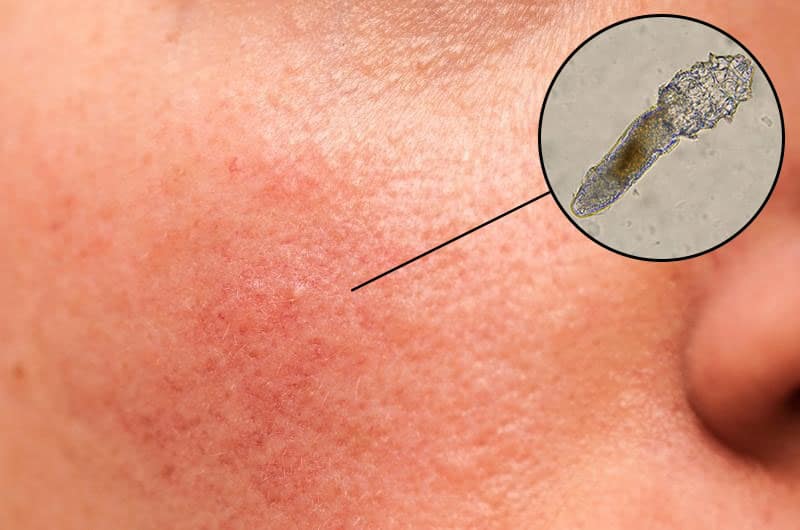
Every person has microscopic mites on their face, called Demodex mites which vary in size from 0.1 mm to 0.4 mm long. They are commonly found on the face in hair follicles, oil glands, and eyelid glands. Some studies found that rosacea patients have a higher density of face mites in the involved areas, and it was suspected that Demodex may produce small amounts of bacteria that rosacea sufferers are more sensitive to, resulting in inflammation. Although scientists haven’t fully identified that mites are the cause of rosacea, it can be a contributing factor.
Rosacea treatment in Singapore often focuses a lot on overhauling a person’s skincare routine, because what a person puts on their face can trigger rosacea flares. Although skincare products do not cause rosacea per se, skin barrier destruction is a side effect of rosacea and skincare can either contribute to worsening flares, or reduce inflammation. It is also found that patients with rosacea had reduced skin surface hydration levels and abnormal oil production because of the dysfunctions of skin barrier, and this may also contribute to the growth of papules/pustules or even Demodex mites which can aggravate flares!
Makeup can also increase the sensitisation of the skin to developing a flare, mainly from the addition of agents that can cause excessive oil production such as mineral oils added in cosmetics. The thick or occlusive nature of some base products, such as primers or foundations, can also be difficult to remove. The excessive cleansing or friction on the skin to remove makeup can further aggravate the skin barrier without a proper skincare routine that is suitable for the rosacea sufferer. A study found that removal of make-up almost every day had a positive relationship with the development of rosacea.
Fairer people do have an increased risk of rosacea, possibly because of the lack of protective effects of melanin against ultraviolet radiation (an exacerbating factor for rosacea). Sun exposure can often cause a rosacea flare because UV light stimulates inflammation within the skin; that’s the reason why sun protection should always be used (At least SPF30)! Unfortunately, rosacea sufferers can also be sensitive to sunscreen ingredients, so a consultation is important when undergoing rosacea treatment in Singapore.
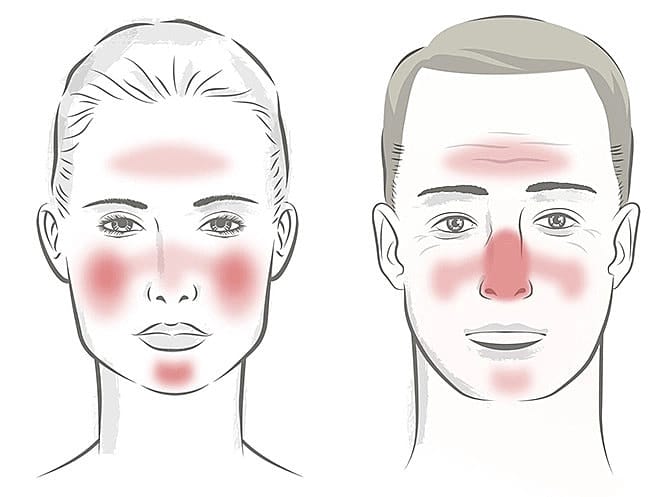
What causes rosacea in different individuals can also be affected by gender and age! For example, the males suffering from rosacea is more likely to have rhinophyma – bulbous tissue growth around the nose – which rarely presents in females. Younger rosacea sufferers will tend to have more flushing and erythema, and older sufferers may have more of telangiectasias, which are dilated or broken blood vessels located near the surface of the skin also known as ‘spider veins’. It is usually said that rosacea is usually more common in women more than men, but that can be due to reporting of symptoms. Females are three times more likely to report rosacea-like symptoms and seek treatment compared to males, giving the assumption that rosacea happens in females more than men.
Can diet and what you put into your body cause rosacea? The answer is a straightforward yes. While individual triggers may vary from person to person, diet consistently plays a strong factor in being a reason for rosacea flares. One National Rosacea Society (NRS) survey in 2002 involving 1,066 rosacea sufferers reported that the main triggers for rosacea were alcohol (52%), spicy foods (45%), certain fruits (13 %), marinated meats (10%), and certain vegetables (9%). Foods rich in histamines trigger inflammatory processes. So, it’s no wonder that we often see ‘alcohol’, especially red wine, ‘dairy products’, or ‘processed foods’ on the list of most common inflammatory foods, as those are foods high in histamines.

Sensory nerves and skin cells (keratinocytes) also contain receptors called TRPV1. When these receptors are activated, they release Substance P and calcitonin-related-peptide (CGRP) which results in an inflammatory response: Dilating blood vessels, flushing, and swelling. It is found that spicy foods, hot drinks, vanilla, cinnamon, chocolate, and caffeine can trigger TRPV1; hence, avoiding some of these foods can help prevent rosacea flares. High blood glucose levels have been found in patients with rosacea, showing a link between overly sugary foods and rosacea which can possibly lead to increased inflammation and rosacea exacerbations.
The link between smoking and rosacea is still not fully proven. There are some studies which show that the risk of developing rosacea significantly increases within 3 to 9 years after a person quits smoking and continues even until 30 years; however, there are actually some studies which find that smoking showed a decreased risk of developing rosacea! What we do know is that smoking can increase the level of inflammation in the body and reduce immunity, which are some of the hallmarks of rosacea. Avoiding smoking may be a good choice to prevent rosacea flares in the long-term.
What also causes rosacea is also allergies involving the skin such as contact dermatitis. When the skin comes into contact with an ingredient that can cause a sudden allergy trigger, the dryness, scaliness, burning, and itching can appear, which is common in rosacea sufferers. Erythematotelangiectatic rosacea (ETR) severity also increased when there was the presence of other allergies such as allergic rhinitis or allergic conjunctivitis.
Interestingly, a study of rosacea in Chinese patients actually showed a higher frequency of previously using anti-allergy products before a clinical diagnosis of rosacea! This might not actually be due to allergies itself causing rosacea, but as a result of the skin condition. Since rosacea sufferers may have symptoms of watery eyes and itching or burning sensation of the skin before the full onset of the disease – commonly known as ‘pre-rosacea’ or ‘early-onset rosacea’ symptoms – a person may look for anti-allergy products to relieve their symptoms, thinking that rosacea symptoms were actually from an allergy reaction.
Some researchers think that rosacea is a neurovascular disorder instead of an autoimmune disorder because of the involvement of blood vessels (flushing, redness, broken spider veins). This is because blood vessels, the ‘vascular’ portion of the disease, often undergo changes when triggered by temperature. With heat stimulus, rosacea-affected skin has a lower heat threshold and enhanced perception of heat compared to those who do not experience rosacea, causing even faster changes to the blood vessels of the face.
There is also something called ‘neurogenic rosacea’ which is a subtype of the 4 main rosacea subgroups. This type of neurogenic rosacea is associated with neurological symptoms like Raynaud’s syndrome, migraines or headaches, and rheumatologic disorders. Some physicians also speculate that the redness and flushing of rosacea symptoms involve the nervous system because rosacea is often either triggered or aggravated when patients are under emotional stress.
Stress is known as the silent killer of the 21st Century, but can it also be a cause for rosacea? It’s interesting that patients with rosacea were shown to have a larger number of critical life events which were identified to be stressful in the ages of early, mid, and late adulthood compared to those who do not have rosacea! In fact, they experienced those critical life events mostly in middle adulthood before the occurring of the first symptoms of rosacea, and having an increased stress intensity with a number of critical life events is significantly related to higher severity of symptoms. The subjective assessment of their stress, identified by feelings of ‘challenge’, ‘danger’, or ‘loss’ can actually be related to worsening of symptoms as well.
So while we can address some of these causes of rosacea, like having good stress management and using the right skin care products, there are some things we can’t change like our genetics and ancestry. Identifying which causes we can address and which we can’t can help to direct a clearer treatment path for your rosacea symptoms. If you’re having difficulty identifying what causes your rosacea, have a chat with one of our professionals at SL Aesthetic today to achieve clarity!
Like what you read? Share them!